Facial Tumors
- Home
- Facial Tumors
Predominantly, it consists of jaw tumors, cysts, and oral cancer.
Jaw Tumors and Cysts
Jaw tumors and cysts are relatively rare growths or lesions that develop in the jawbone or the soft tissues in the mouth and face. Jaw tumors and cysts—sometimes referred to as odontogenic or nonodontogenic, depending on their origin—can vary greatly in size and severity. These growths are usually noncancerous (benign), but they can be aggressive and expand, displace or destroy the surrounding bone, tissue and teeth. Treatment options for jaw tumors and cysts vary, depending on the type of growth or lesion you have, the stage of growth, and your symptoms. Mouth, jaw, and face (oral and maxillofacial) surgeons treat jaw tumor or cysts, usually by surgery, or in some cases, by medical therapy or a combination of surgery and medical therapy. Some lesions commonly seen in clinical practice are as follows:
- Ameloblastoma: This rare, usually noncancerous (benign) tumor begins in the cells that form the protective enamel lining on the teeth. It develops most often in the jaw near the molars. The most common type is aggressive, forming large tumors and growing into the jawbone. Although this tumor can recur after treatment, aggressive surgical treatment will typically reduce the chance of recurrence.
- Central giant cell granuloma: Central giant cell granulomas are benign lesions that grow from bone cells. They most often occur in the front portion of the lower jaw. One type of these tumors can grow rapidly, cause pain and destroy bone, and has a tendency to recur after surgical treatment. The other type is less aggressive and may not have symptoms. Rarely, a tumor may shrink or resolve on its own, but typically these tumors require surgical treatment.
- Dentigerous cyst: This cyst originates from tissue that surrounds a tooth before it erupts into the mouth. This is the most common form of cyst that affects the jaws. Most often these cysts will occur around wisdom teeth that are not fully erupted, but they can also involve other teeth.
- Odontogenic keratocyst: This cyst is also referred to as a keratocystic odontogenic tumor because of its tumorlike tendency to recur after surgical treatment. Although this cyst is typically slow growing, it can still be destructive to the jaw and teeth if left untreated over a long period of time. Most often the cyst develops in the lower jaw near the third molars. These cysts may also be found in people with an inherited condition called nevoid basal cell carcinoma syndrome.
- Odontogenic myxoma: This is a rare, slow-growing, benign tumor that occurs most often in the lower jaw. The tumor can be large and aggressively invade the jaw and surrounding tissue and displace teeth. Odontogenic myxomas are known to recur after surgical treatment; however, the chances of tumor recurrence are typically lessened by more-aggressive forms of surgical treatment.
- Odontoma: This benign tumor is the most common odontogenic tumor. Odontomas often have no symptoms, but they may interfere with tooth development or eruption. Odontomas are made up of dental tissue that grows around a tooth in the jaw. They can resemble an oddly shaped tooth or can be a small or large calcified tumor. These tumors may be part of some genetic syndromes.
- Other types of cysts and tumors: These include adenomatoid odontogenic tumor, calcifying epithelial odontogenic tumor, glandular odontogenic cyst, squamous odontogenic tumor, calcifying odontogenic cyst, cementoblastoma, aneurysmal bone cyst, ossifying fibroma, osteoblastoma. central odontogenic fibroma and others.
Oral Cancer
Oral cancer (mouth cancer) is the broad term for cancer that affects the inside of your mouth. Oral cancer can look like a common problem with your lips or in your mouth, like white patches or sores that bleed. The difference between a common problem and potential cancer is these changes don’t go away. Left untreated, oral cancer can spread throughout your mouth and throat to other areas of your head and neck.
Approximately 63% of people with oral cavity cancer are alive five years after diagnosis.
Oral cancer includes cancers of the mouth and the back of the throat(oropharynx). Oral cancers can develop under the following subsidies:
- lips.
- gums.
- The lining of the inside of your cheeks.
- Anterior 2/3 of the tongue.
- The floor of the mouth (the part under your tongue).
- The palate, Roof of the mouth.
- Retromolar Trigone Area, The area right behind the wisdom teeth.
- Oral cancer most often occurs in people over the age of 40 and affects more than twice as many men as women. Most oral cancers are related to tobacco use, alcohol use (or both), or infection by the human papillomavirus (HPV).
Symptoms:
If you have had any of these symptoms for more than two weeks, see a specialist in oral and maxillofacial surgery.
- A sore, irritation, lump or thick patch in your mouth, lip, or throat.
- A white or red patch in your mouth.
- A sore throat or a feeling that something is caught in your throat.
- Difficulty chewing, swallowing or speaking.
- Difficulty moving your jaw or tongue.
- Swelling of your jaw that causes dentures to fit poorly or become uncomfortable.
- Numbness in your tongue or other areas of your mouth.
- Ear pain.
Diagnosis is achieved with the help of battery of tests that include one or more tests such as clinical examination, usg of neck, biopsy, naso-pharyngoscopy, CT SCAN, MRI, and PET scans.
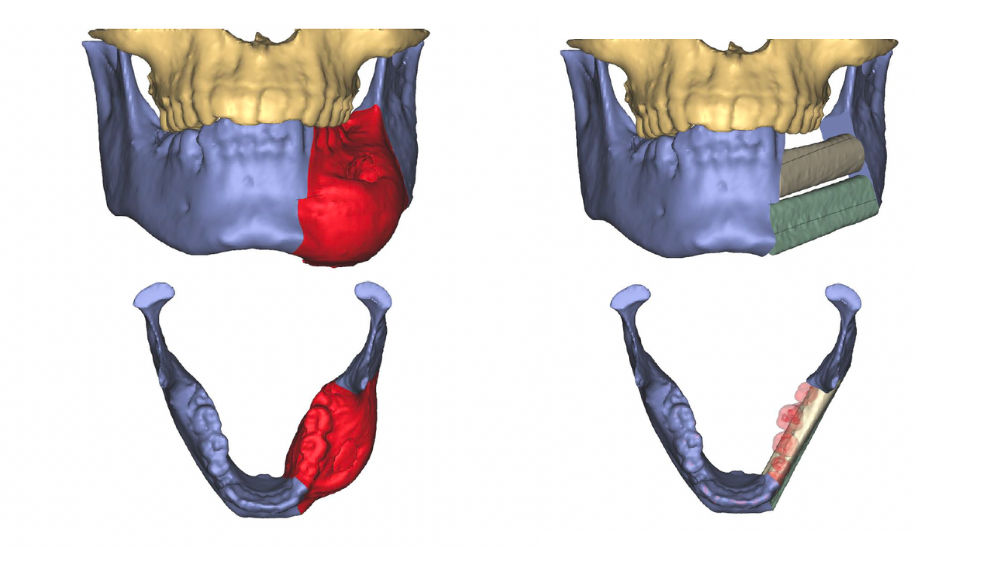
Post establishment of diagnosis, the case is presented to a multidisciplinary tumor board and a definitive treatment plan is planned and executed. The mainstay of treatment includes surgery and reconstruction (microsurgery-free flaps), along with chemotherapy and radiation. In reconstruction, we use microsurgical free flaps as a routine method of reconstruction. The most commonly used flaps are: Radial Fore Arm Free Flap( RFFF), Anterolaral Thigh Flap (ALT), Medial Sural Flap (MSAP), Fibula Osteocutaneous Flap (FOSC), and Deep Circumflex Illiac Artery Flap (DCIA). We use MDT protocols along with state-of-the-art techniques( CAS, Intraoperative Navigation, etc.) in the management of these tumors. The goal is curative intent and to provide the best functional (speech, stomatognathic ) and aesthetic outcome.

Facial Tumors FAQ
General Question
Maxillofacial Surgery can be overwhelming. Whether you’re scheduled for your very first oral surgery, or you’ve undergone oral surgery before, you probably have several pressing questions for your Maxillofacial surgeon.
Any swelling (lump) or non-healing ulcer in the jaw or oral cavity that has not healed beyond 3 weeks is a sign for concern and has to be consulted with the specialist.
There are two types of tumours: benign and malignant, which have to be diagnosed by a specialist.
Ulcer/sores in the oral cavity /lips that doesn’t heal around 2-3 weeks, and bleed easily.Roughspots or crusty areas on the mucosal lining of oral cavity, numbness pain in face, neck oral cavity without any cause, swallowing, speech, jaw movements difficulty, earache,long standing bad breadth and weight loss.
SMOKING,BETEL NUT AND GHUTKA, EXESSIVE ALCOHOL, SPICEY FOOD, SHARP TEETH(THAT CAUSES MUCOSAL TRAUMA),INFECTIONS LIKE SYPHILIS-HPV VIRUS AND FAMILY HISTORY
Clinical examination, biopsy, and radiological investigations such as CECT, MRI, PET CT, USG, / blood examination are the modalities for diagnosis and workup.
Surgery, chemotherapy, and radiotherapy are the methods of treatment.
Technology and surgical refinements have improved the outcomes in the present-day scenario. The state of techniques like CAS and microsurgery has changed the outcomes so that patients can be rehabilitated as much as possible to their pre-surgical status so that their stomatognathic functions like speech, swallowing, and facial cosmesis are well maintained and they will not be oral cripples.
It’s better to visit as early as possible when one notices an ulcer or swelling. Early detection helps in almost complete cure rather than late advanced stage presentation.
Book Now
Make An Appointment
Open Hours
- Mon – Sat : 10 AM to 02 PM
- Mon - Sat : 04 AM to 08 PM

